Over the last few weeks, I have been asked by many people—from patients and fellow healthcare professionals, to family and friends—what my advice would be about taking the newly approved COVID-19 vaccines?
I’ve read the data behind the trials that have concluded effectiveness, to the extent that data has been released so far. I am going to share my thoughts here and what I have been advising people.
Firstly, right off the bat, barring an imminent life-or-death situation, I do not believe in ever telling (read “telling” in italics) my patients what to do, or treating them like they are stupid. I believe in presenting the evidence to them and letting them decide what they want. More often than not, my patients will ask me what I recommend, and then I’ll give them my opinion to either act on, or not.
The vaccine data so far, does suggest efficacy in protecting against COVID-19 in the expedited trials. However, when you look at the published information and read the paper, the numbers of total cases detected, were but a very small percentage in both the vaccine (Pfizer) and the placebo arms of the trial. Even in the placebo group, only 0.7 percent of around 22,000 people were diagnosed with COVID-19, in the primary endpoint time reported. 99.3 percent of people were not. In the treatment group who were given the vaccine, the numbers diagnosed with COVID-19 were indeed significantly less than this, closer to 0.05 percent. It appeared to be well-tolerated with few adverse effects.
As for certain groups, the vaccine was not tested in pregnant or lactating women, or children under the age of 16.
Here are my 3 questions:
- How long is the immunity expected to last? The trial was only able to report data for around 90 days after the first dose. What about when COVID-19 mutates and a new strain comes along?
- The median age of trial patients was 52. And only 21 percent (1 in 5) had at least one underlying comorbidity. How will the vaccine effectiveness translate into the over 70s and more vulnerable, the vast number of whom constitute hospitalizations and deaths? The majority of patients I’ve seen hospitalized are usually much older than 50 and have a number of other chronic illnesses.
- Will this have any effect on asymptomatic spread (the vaccine manufacturers have already said it is unlikely)?
I have more concerns over the true efficacy of this vaccine, than I do of its safety—especially with a virus that’s got a very high asymptomatic rate.
Having said that, I tailor my advice at this early stage according to anyone’s individual risk profile and circumstances.
I’ve noticed that high-risk groups, including the elderly and frontline healthcare professionals (many of whom are family and close friends)—seem more willing and keen to take the vaccine immediately. I advise anyone who wants to get it, and especially if they are in a high-risk group, to GO AHEAD.
As a personal example, my mom and dad are both eager to get it, and I am advising them to proceed. My 30-year old healthy cousin who is already more hesitant, I am not going to get in her face and tell her it’s imperative to get it ASAP. I simply do not have the data to do that with confidence. Do you have diabetes, obesity, COPD, or live with a vulnerable person? Probably more reason to get it.
Remember, with any vaccine rolled out to millions of people, there will inevitably be some side effects reported (and you will hear about these no doubt online). And if you do get it, whatever you do, don’t let your guard down and assume you can no longer get sick. Even the trial only followed people for 3 months!
I am not on board though with some physicians I see on news and social media, virtually acting like salesmen and women for the vaccine, including making rather bold statements about the vaccine “ending” COVID. Best advice is all we should be giving based on the facts of where we are. Nobody—not even Dr Fauci or any lifelong academic who sits in a lab all day—can possibly know yet how this will pan out in the real-world general population. Considering not one of us had even heard of COVID-19 a year ago—there are an awful lot of experts out there who seem to know a lot more than they possibly could. It’s all just predictions, projections, and unfortunately for science—a lot of emotions too. It’s understandable how much people want this disaster we’ve faced over the last year to come to an end, and see this as a glimmer of hope. But it’s important we stay level-headed and realistic.
As for me personally, in the interests of full disclosure, even if I hadn’t already had COVID-19 earlier this year—I would still have waited a few months before getting the vaccine to observe its effects and be absolutely sure it’s something that will help (ultimately, how many vaccinated people still end up getting COVID over time?). That’s a personal choice, but not my advice to everyone per their risk profiles. To be clear, I believe in vaccinations—recommend the usual ones to my patients including influenza, hepatitis, measles, rubella, typhoid etc. But those are for known diseases that have been circulating among humans for hundreds, if not thousands, of years. For me, “science” is not making a vaccine and doing a single trial. Science is seeing it actually work in real life. Millions will be getting it, so we’ll know soon enough. And I’ll share that data with you when we have it.
I hope to God the COVID vaccine proves a staggering success and helps end the pandemic—but I wouldn’t be the least bit surprised if like the Flu virus, it didn’t end anything—and simply enabled us to be more comfortable living with it. And as far as rays of hope go to return life back to normal, that is still something to aspire to.
—Suneel Dhand, MD
 Suneel Dhand is a physician, writer, and YouTuber. He is Founder at MedStoic Lifestyle Medicine and DocsDox . Follow him on YouTube and Instagram
Suneel Dhand is a physician, writer, and YouTuber. He is Founder at MedStoic Lifestyle Medicine and DocsDox . Follow him on YouTube and Instagram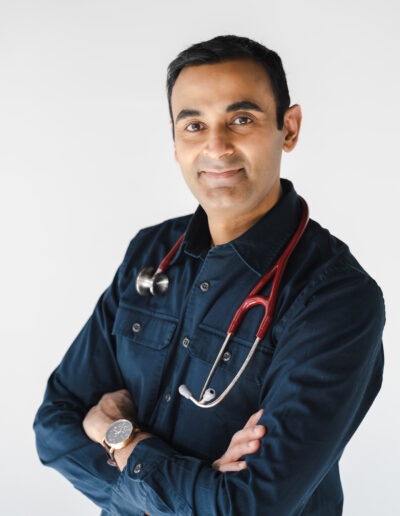
So here’s the risk-benefit equation:
Sickness or death from COVID-19 vs. a sore arm and maybe it wears off over time or there’s some as yet unknown long-term risk factor that NO ONE has predicted.
Seems pretty obvious to me!
I got my shot last week and happy to do it.
Hi Andrew, broadly agree with this fundamental analysis– however I do also have a lot of healthy younger patients, and even relatives, who are in unique situations e.g. females trying to get pregnant, in whom the advice is a bit more cautious right now. Regards, Suneel
I totally agree, I am also planning on the wait and watch approach. I am really surprised to see some of the so called ‘elite health care professionals’ vouching that this is the ‘magic bullet’ for COVID, a very unscientific approach in my opinion.
Thank you.
Pramo, I completely agree. Many, many doctors I know (but not the ones you see on the media) are of course happy with a potential successful vaccine– but acknowledge that this will not “eradicate” COVID, any more than the Flu vaccine has eradicated Influenza. Regards, Suneel
Thanks for this analysis.
Hi Jo, welcome! Suneel
Interesting analysis. In my country, Italy, the government is supposedly thinking about the hypothesis of making the vaccine mandatory for health care workers, in order to decrease the novax movement resistance (apparently not a large percentage of doctors and nurses is keen on getting the vaccine soon).
Hi Luigi, thanks for your message, that’s interesting to know. I would have expected in Italy, there to have been a very small “anti-vax” movement. I am not anti-vax, but wanting to wait a few months, is something I understand anyone wanting to do (in the USA, they are not mandatory…yet). Regards, Suneel
I had covid in July 2020. I am 57yrs old and no known healthy issues. My employer is making the vaccine mandatory for all. I DONT want to get it, but don’t see any other option. Which vaccine would you recommend for me to get?
I am a ginec-obst with 69 years and more then fourty years of practice and learned a lot reading you.wait for three or four months and then decide will be my strategy and meanwhile being careful and masked….
Thanks for your considerations.
Hi Pedro. I appreciate you reading my work, and yes, make your own informed decision and be careful! Best Regards, Suneel
I am 82, appreciate your analysis of the health benefit of accepting the covid-vaccination. It is for the reasons that this pandemic, a new phenomenon of global significant that might lead to a lost of lives in the magnitude of the plague, MEDITERRANIAN flu, small-pox etc. It is seemingly all the opinion of the promotion in favour of vaccinations to attenuate the the consequence of infection of Covid-virus, are a matter of person choice. I am in favour of taking the vaccination for reason, that my acceptance to be subject of an medical agent that is still on trial, contribute a data point to this present pandemic. I am most grateful for your awareness to share with the general public, your professional knowledge and skill.