One of the topics that I’ve written about most on my blog, is maintaining the human connection in medicine, and never forgetting that solid communication is at the core of all we do in healthcare. Pre-coronavirus, the main barriers I saw to this were shrinking face-to-face time with patients, burdensome electronic medical records, skyrocketing bureaucracy, and a lack of educational reinforcement among all medical professionals.
Communication skills, including active listening and displaying empathy, are very teachable to anyone. While you can probably never turn a bad communicator into an amazing one—each one of us can always go up a few rungs on the skills ladder. All it requires is motivation and the right message. Human communication is, after all, a fascinating science—that we are all at the mercy of, even if we don’t realize it.
That being said, here are my 3 fears for how coronavirus has negatively impacted communication and humanity in medicine:
1.Telemedicine
There’s little doubt that the coronavirus crisis has resulted in what was a slow growing movement towards telemedicine, being launched into the stratosphere. Nobody who wrote this article about an embryonic industry in 2019, could have predicted what was going to happen in 2020! I have seen this unfold before my very eyes as a hospital medicine doctor, with patients telling me all about their telemedicine appointments with their primary care doctors and specialists (something I’d never heard before March). Data shows almost 50 percent of physicians now see patients via telemedicine! However, humans will always be humans—and healthcare being a uniquely emotional arena—means that telehealth won’t quite make the cut for many people. I’ve already heard from physician colleagues telling me that as soon as their clinics have reopened, patients are coming back to meet with them in droves, despite having an easy video option available at the click of a button! This doesn’t surprise me at all, and although I don’t doubt telemedicine will play big role in the future—there’s a lot of people who crave that human connection when it comes to serious issues related to their health.
2.Masks
Although there was a lot of initial debate about whether masks needed to be worn by everyone in hospitals, it now seems to be a near-universal policy not just in hospitals, but in outpatient clinics too. When we are communicating with another human, so much of that relies on facial expressions and reading emotions. This is almost impossible to do if a patient is wearing a mask, and likewise for a physician to express compassion, empathy, and communicate well—if the patient can’t see their face! Not to mention that a huge percentage of elderly patients already struggle with hearing, and need to be able to partially lip read. I’d like to see a way around this, even if it involves sitting several feet away and talking like humans, and then only donning masks when examining perhaps? I hope we can somehow avoid having important conversations wearing them. Over the last few months, I’ve not felt quite right in hospital—especially during times when families have been coming in for terminal care discussions or seeing their gravely ill loved one, that I’m talking to them with my face covered. It’s just not something human beings are built to do.
3.Hospital policies for families
Since the pandemic begun, healthcare facilities have become extremely strict about allowing patients’ loved ones to visit them. I have written and spoken about this issue previously, and believe that some of the policies were unnecessarily harsh, particularly in the case of terminally ill patients. Think about it: the ritual of being at the bedside of an ailing loved one, is something that goes back to caveman days. It’s as old as humans have been on the planet. Imagine the person you love most in the world, lying in a hospital bed alone—and you couldn’t see them. Hospitals are now slowly relaxing this policy, and I hope that a day will come in the not-too-distant future when I walk into the room of a beaming 90-year-old patient, surrounded again by his children and grandchildren. Nothing could be more human than that sense of relief, of someone surrounded by the love and support of their family, at a time when they are down.
Medicine is about humanity. Our internal needs and what we respond to, are not going to change because of COVID-19. We must find a way to keep the human connection at the core of all healthcare. Social distancing and covering our faces may serve a purpose. But even outside of the hospital, are we not going to help that elderly lady who falls over in the street? The middle-aged man who collapses in the restaurant? The semi-disabled person who needs help carrying their bag at the airport? Don’t let this dastardly virus not make you human anymore.

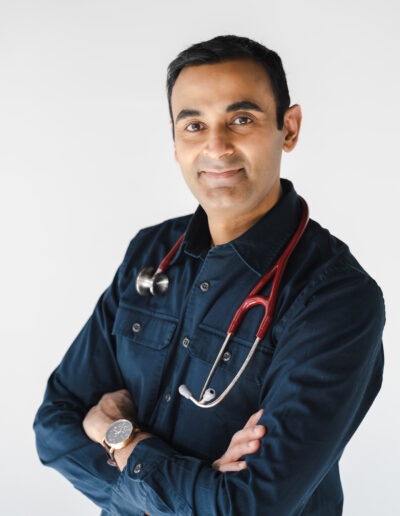
Suneel Dhand is a physician, writer, and YouTuber. He is Co-Founder at DocsDox. His two main passions are preventive medicine and improving communication skills. Follow him on YouTube and Instagram.
Bravo!
It needed to be said Suneel but how many medical professionals can see the trees for the forest?
I would add to your commentary by citing the need for doctors, dentists and others that deal directly with patient care to make a living. Those that do not have salaried positions have suffered financial losses and, I am sure, are willing and needing to make up for lost income. Telemedicine is a way to go.
I had a telemedicine visit with my internist about a week ago. When I looked at the charge to my insurance company for maybe a 15 minute call it was $249! Obviously Medicare Advantage saw fit to only pay $83.00 but what happened to the difference? I, the patient who is paying for this (even through insurance), don’t have a clue about the charge and payment.
Another reason for a loss of connection and humanity.
If that isn’t alienating, I don’t know what is.